Two hospice leaders on the value of art therapy
Opinion
Dr Ros Taylor MBE, Medical Director at Harlington Hospice and the Michael Sobell Hospice
Every team in a hospice works differently, but I think if you are going to pursue the mission of palliative care and explore total suffering or total pain, then an art psychotherapist is worth the investment.
Can you tell us a bit about your hospice?
We support people both in their homes and within our inpatient hospice. We support adults and children before a death and after an adult’s death. We find children cope with loss better if that loss is anticipated and they build a trusting relationship with an art psychotherapist before the death.
Our art therapy team is doing formal research in neurodiversity, particularly in how children living with neurodiversity cope with grief, and they are becoming recognised for their expertise in the area.
Why do you offer art therapy?
I’ve been a palliative care doctor for about 35 years, looking after people as they are approaching the end of their life and trying to explore with them what matters at this critical time. I’d never worked with art psychotherapists before the last few years of working at Harlington Hospice, but working with our art therapy team has been revelatory.
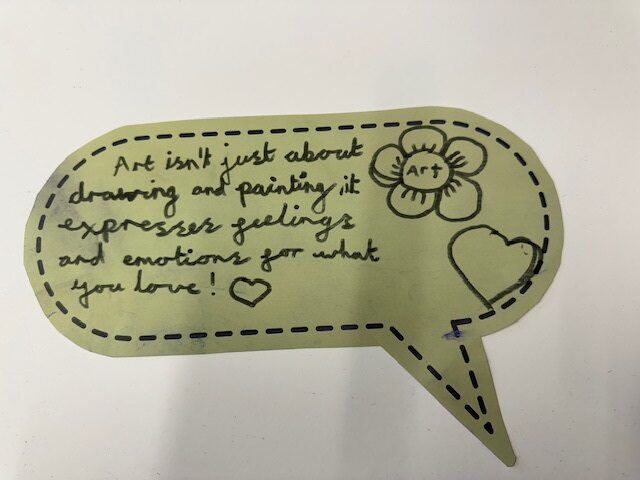
What I’ve seen is that art psychotherapy brings a new medium for communication. Doctors and nurses and maybe traditional psychotherapists are very good at using language to explore what is of major concern to a patient, a family or a child. But words often aren’t enough.
Pain often has a physical cause, particularly in advanced disease, but there are many components to that pain and suffering. Often, on a busy hospital ward, we only look at the physical, whereas what is actually causing a lot of suffering is facing loss, leaving people behind, losing identity and social losses. I think art psychotherapy is a tool to get to the heart of that total pain or suffering. Even if somebody is bed-bound, they can still use art materials, look at pictures, draw, often paint, even when their body isn’t working very well.
Our art psychotherapy team – Nana, Paula and Lily – are an integral part of our multidisciplinary team. As art psychotherapists, I’ve heard them give such important insights into family dynamics because of their creative work at the bedside. We’ve even seen the team discover really important insights when the patient is delirious or confused, or maybe talking about their dreams or maybe even hallucinating. From my perspective, it’s about looking at communication in a different way and probably at a deeper level than many of our conversations as doctors and nurses.
What are the challenges?
The main challenge is about communicating that we have an art psychotherapist in the team and explaining art therapy to a patient, a family or maybe a child and what it means — because it might sound quite scary.
But we have worked with our art therapists, Nana, Lily and Paula to find the words to explain. Often Lily will turn up at the bedside with a basket of creative things to explore or look at – and they are masters at gaining rapport with people.
With financial pressures on hospices, why continue offering art therapy?
All hospices are facing financial challenges. But there is a risk that if funding focuses on nurses and doctors, then we’re back to just looking at the pure physical, which loses the mission of palliative care.
If we want to get to the heart of emotional and psychological distress, over the last five years I have seen how art psychotherapy has made such a difference. I’ve seen moods lifted. I’ve seen concerns addressed that haven’t been addressed by other people. It’s often allowed us to facilitate a discharge home or even to another country, or to organise weddings!
Could art therapy be more widely adopted in hospices?
Every team in a hospice works differently, but I think if you are going to pursue the mission of palliative care and explore total suffering or total pain, then an art psychotherapist is worth the investment.
Heather Tudor, Chief Executive of Severn Hospice
We are committed to providing person-centred care and art therapy helps us to provide an additional layer of support. It is especially valuable to patients and helps them navigate their individual journey and can help them to live as full a life as possible.
Can you tell us a bit about your hospice?
Severn Hospice provides specialist care for people living with incurable illness across Shropshire, Telford & Wrekin and Mid-Wales. We support around 3,000 patients and their families each year through a combination of inpatient care, day services, outreach in the community and bereavement support. Our approach is holistic and person-centred – we care not only for the clinical needs of our patients but also for their emotional, psychological and spiritual wellbeing.
We are with our patients and loved ones from the moment they are referred to us and for as long as they need us, helping them live as well and as independently as possible within the limitations of their illness.
Why do you offer art therapy?
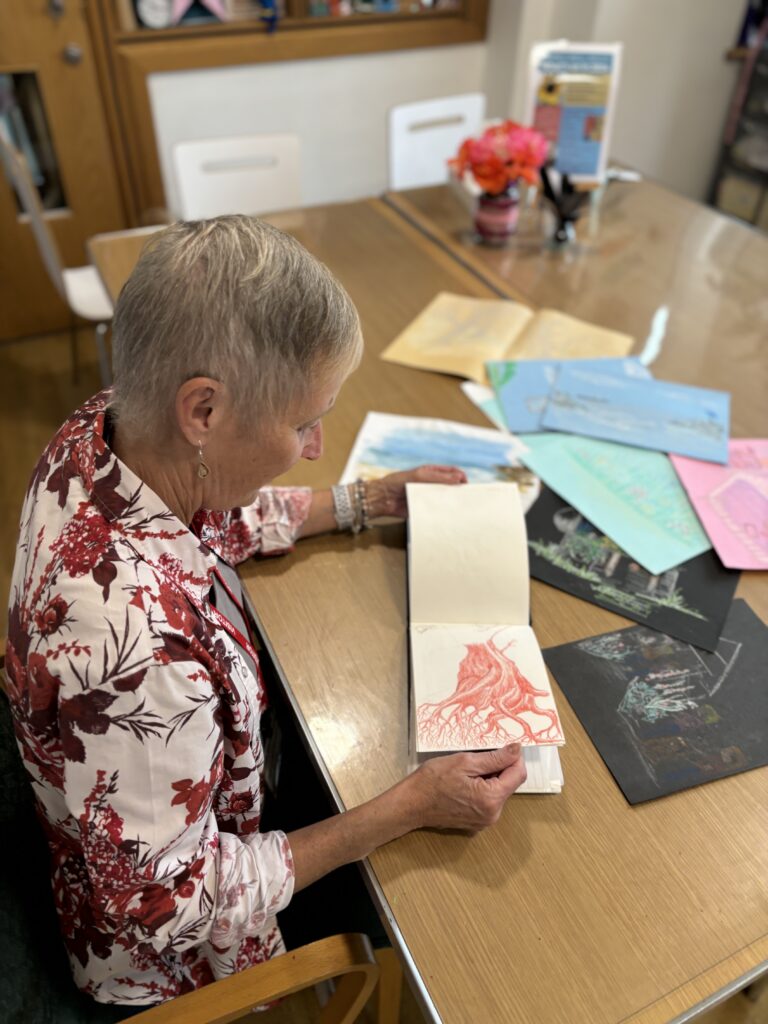
Our art therapy service has a real therapeutic value. Patients have fed back that it has helped reduce anxiety, improved their mood and provided a greater sense of identity. We also see many patients engaging more with activities and general day-to-day life following art therapy sessions.
Art therapy isn’t about the finished image, although many are particularly good. We provide a safe, non-judgemental and supportive space where patients can explore and process their experiences, express and communicate complex emotions and reflect on their journey via art materials, with an art therapist on hand to support them.
For many, it offers a sense of control, a way to process feelings around illness, treatment, relationships and mortality. Art therapy supports the emotional and psychological dimensions of care that are often difficult to address through words alone.
Overwhelmingly patients have found that loved ones do not want to talk about death and dying but this is what the patient does want to talk about. The art therapy sessions allow patients to process these thoughts before perhaps communicating with their loved ones about what they need.
Families gain a deeper understanding of their loved ones’ emotional world, and for some the artwork becomes a treasured legacy.
Patient experience is important to us, and we gather feedback through forms where patients share their experiences and suggest improvements, along with rating how they feel during initial and review sessions. We also receive frequent verbal feedback, with patients often mentioning at the end of sessions that they feel better after talking through issues or creating images related to specific topics. These comments help us understand the value of the art therapy service we provide.
What are the challenges?
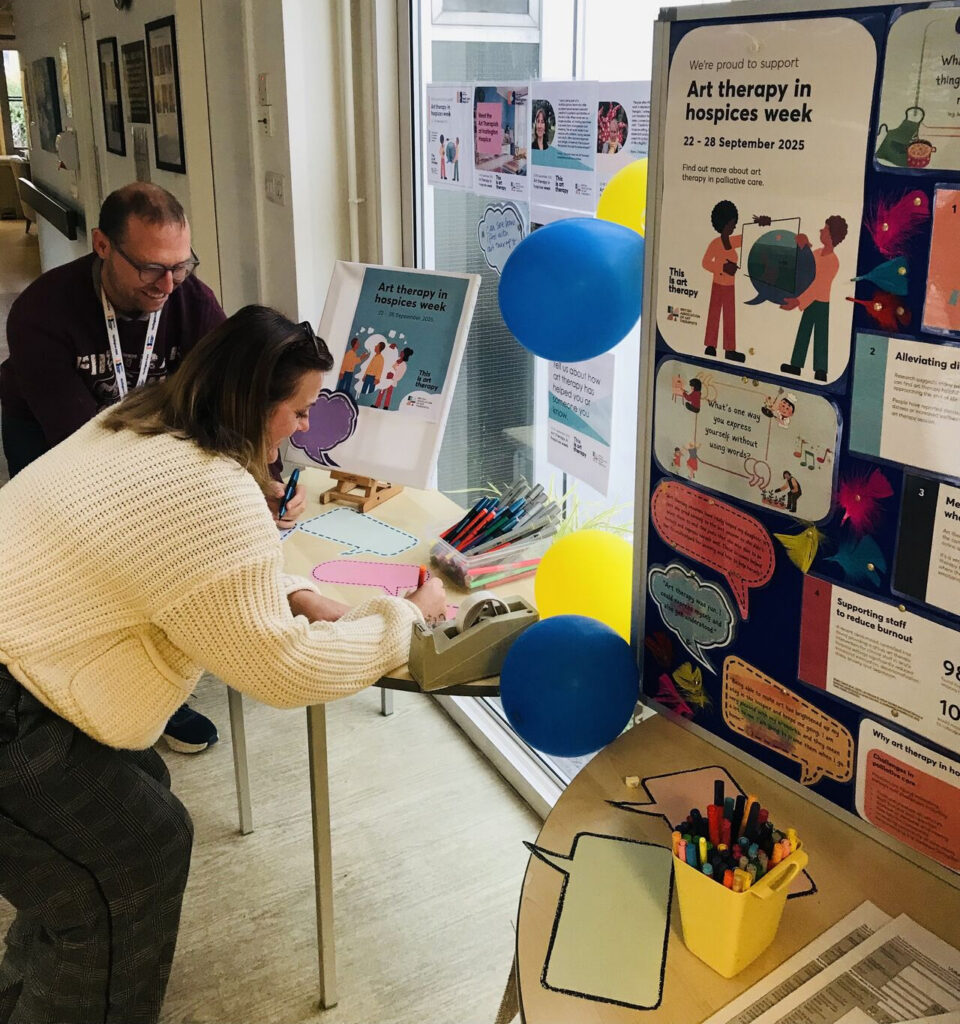
One of the main challenges we face is helping patients understand what art therapy truly is. There’s a common misconception that you need to be good at art, have a creative background to benefit from it, that it is a taught session or you have to talk.
We work hard to shift this perception by making it clear that no prior experience is necessary. You don’t have to consider yourself an artist, or even have an interest in art, to find value in the sessions.
To address this challenge, we’ve created a light and calming space in our hospice buildings and informative leaflets that are shared with patients, and engaged our wider teams through presentations, who then can help raise awareness, confidently explain what art therapy is and recommend patients give it a try. Once they do, many are surprised by how meaningful and comforting it can be.
With financial pressures on hospices, why continue offering art therapy?
Like many hospices, we are facing increased costs and pressure on our funding as supporters cope with the same cost-of-living rises that we do.
We are committed to providing person-centred care and art therapy helps us to provide an additional layer of support. It is especially valuable to patients and helps them navigate their individual journey and can help them to live as full a life as possible.
Art therapy supports the work of our clinical teams and patient and family support social work, pastoral and clinical psychology teams, thus freeing them up to provide other essential services.
It can also help reduce pressures within other departments for example one art therapy patient stopped calling day services so frequently because she felt supported through this intervention.
Our care goes beyond clinical treatment and despite increased financial pressures, we see art therapy as an essential part of care; it is one of the therapeutic ways we can truly care for the whole person. It can provide positivity and acceptance at a time that can feel completely overwhelming.
Could art therapy be more widely adopted in hospices?
Art therapy has enormous potential across hospice settings. It doesn’t need a lot of space – art therapists can set up in a small room or at a bedside with minimal materials.
Understanding the benefits is a good place to start and this can begin by sharing success stories and best practice within the hospice community and our passionate art therapists speaking up about their roles.
More research into the benefits may also open grant and funding opportunities for hospices to introduce this unique and much valued service
Art therapy in hospices