Working as an art therapist with people who experience psychosis
Spotlight
Spotlight is our regular series dedicated to shedding light on the roles of art therapists within different contexts. In this article, Dr Chris Wood tells us about her work as an art therapist with people who experience psychosis.

Who are you?
I have been working as an art therapist for some 40 years. The role is a strong part of who I am.
I think of myself as a practitioner, academic and activist. Although there have been ups and downs, I love the work and the people I walk alongside because of it. Like many people, I was originally drawn to art therapy because it is a way of combining shared human knowledge about worldwide culture and staying alive.
Where I work as an art therapist
I work in the NHS, in educational settings and with the charity Art Refuge. All of them educate me about the episodic and impermanent nature of psychosis. They also help me think about what might be a helpful response when meeting with people who experience it.
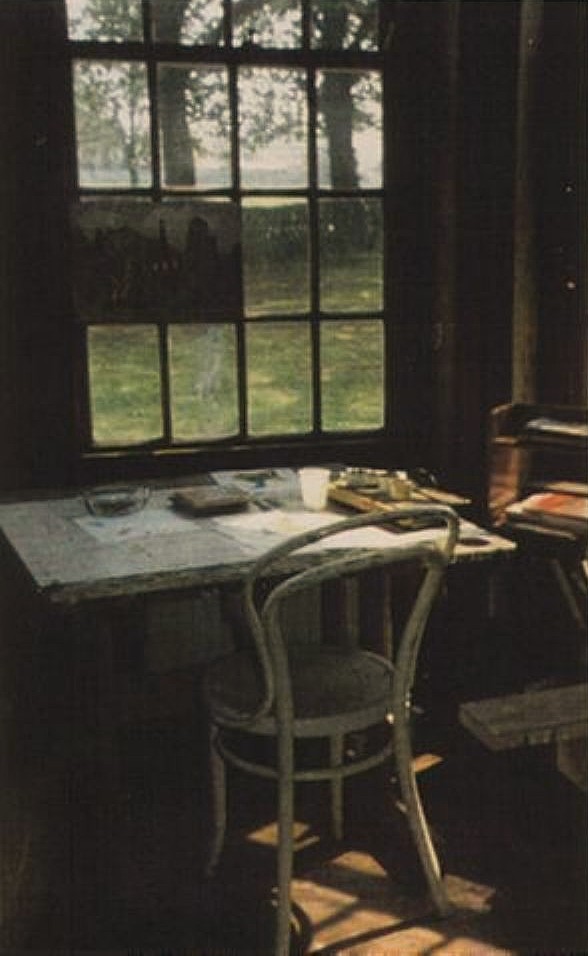
In the NHS, I work with a small team of art therapists in community provision. We receive referrals from people working with inpatients and outreach services. Those who make referrals want the best for the people they refer, but many work in stretched and stressed services. They hope we can offer clients time and a place to think and feel in the lovely old studios where we work. Many staff and clients I meet help steer my moral compass in navigating the work in stretched services.
Getting here
Since being young, I have wondered why people are troubled. I left school as a teenager and worked in a factory. The women I worked alongside on the production line cared for me, and they wanted me to have the opportunities not available to them. There were discussions and humour about what people need at difficult times. Those women helped me decide to study A-levels at night school, and I ended up studying for a degree.
While a student, I heard a talk for the charity Mind, organised by a mental health nurse. I was fascinated by what the talk taught me about how art therapists work, and I decided to train. During my early time at Goldsmiths, I remember Di Waller, who is now Honorary President of the British Association of Art Therapists, convincing me to stay in London to train by telling me that few places could teach me as much about the socio-economic issues underpinning mental health as London. She knew this underpinning knowledge is crucial, but I also wanted, and still want, to explore how we all use our imaginations to find ways to live.
After training, I was lucky to get a post at the famous Netherne Hospital. Many of the clients there experienced psychosis, and this is where my deep interest in it began. The Netherne art therapy studio was part of the admission unit within the hospital, where people would stay for a few months before returning to their lives. There were longer-term patients in other parts of the 1000-bed hospital, and in what I saw of their lives, I witnessed the consequences of living in a psychiatric hospital for many years. I also saw how afraid people had been to ask for help because of prejudice and stigma.
I have long sought out ideas about how to respond when meeting with a person who has episodes of psychosis. I have followed additional training, research, relevant organisations and conferences. I have learnt about the Hearing Voices Movement. Along the way, I have written a PhD and articles about art therapy, psychosis and service user movements. Many people have helped me learn my craft, especially people I have worked alongside who experienced psychosis.
A typical day at work in the NHS
I work alongside art therapy colleagues and students. Our studios are in an old building, but we make them welcoming. We respond to referrals from all NHS disciplines.
Many people who come to meet us have experiences of psychosis. We offer initial meetings, and in discussions with the clients we decide how to use the art therapy. These first meetings are followed by individual or group sessions.
When meeting clients, I think with them and colleagues about what they might need and how to show respect. We are conscious that we all need a sense of safety, connections with others and the wherewithal to live, so from the beginning, we think alongside clients about the things that support them in their lives.
We also ask clients repeatedly about what touches their imagination. The suggestions we might offer about building, drawing, writing, photography, watching or listening are informed by what they say. Sometimes, finding confidence in their imagination takes them a little time. Time absorbed in artmaking seems to help recover the capacity to think, and clients often notice this themselves.
We have found ways to work briefly in response to stretched mental health services. This has meant that we increasingly look to the client’s sense of what is important and what they feel they can manage. I am always humbled by how much clients in groups help each other and how they can share lived experiences in potent ways.
At the end of groups, we offer several signposting sessions. We travel with clients to visit galleries, third-sector groups and service-user meetings. Clients of one former art therapy group established a monthly support group, which is inspiring
What I love about what I do
I love working alongside people and watching them imagine new possibilities in what might be difficult lives. I know that people in the middle of a psychotic episode might find it hard to relate to others, but they may be able to share quietly while they make artwork. Eventually, they might find the confidence to speak. So, the very nature of art therapy gives people the option of being in sessions without necessarily needing to speak at first. This helps them engage at their own pace.
After being part of a day-long workshop, a person of 50 experiencing episodes of psychosis since their teens stunned me by saying:
I did not know people could talk about these conditions in the way people have done today.

How I look after myself in my role
I talk with colleagues. I think using supervision. I try to absorb myself in things that bring me joy outside work: friends, the cultural world (including popular culture), yoga, the countryside, reading stories and writing. I join campaigns.
What I wish I had known when I started
I wish I had done more with others to campaign to protect services from the ravages of austerity. Also, that I had known more about how we all have public and personal agency and how good public services, given funding, might still provide a valuable, secure base for people.
Moving forward
I have been inspired by the story of Maggie’s Centres, which provide free holistic cancer care. When I look at beautiful buildings now, I can imagine some (with art therapy studios) dedicated to mental health.

Our upcoming courses with Chris
Chris will be teaching courses for art therapists to develop their practices in working alongside people experiencing psychosis. Find out more about our:
Read more
To learn more about art therapy for people experiencing psychosis, you can read our evidence page and guidance on art therapy and psychosis:
You might also be interested in reading these articles by Chris published in our journal:
- Acceptance in the Hearing Voices Movement: how might this be relevant for art therapy service-users? (2020)
- Art therapy with people diagnosed with psychosis: therapists’ experiences of their work and the journey to their current practice (2021)
