Working as an art therapist in NHS paediatric rheumatology
Spotlight
Spotlight is our regular series dedicated to shedding light on the roles of art therapists within different contexts. In this article, Dr Patricia Watts tells us about her work at the Teapot Trust as an art therapist working with children in hospital.

Who I am
I qualified as an art therapist in 2007 at Queen Margaret University, Edinburgh. Before training, I attended art school, where I studied Fine Art, specialising in drawing and painting. Since qualifying as an art therapist, I have worked with children and young people across a range of voluntary sector settings.
Where I work as an art therapist
The majority of my clinical work is with Teapot Trust, a charity specialising in art therapy for children and young people living with long-term physical health conditions. In this role, I am embedded within the Paediatric and Adolescent Rheumatology Service at the Royal Hospital for Children, Glasgow, where I have worked since 2015.
Getting here
Paediatric rheumatology was a new area for me. My background was in homelessness and trauma work, and joining Teapot Trust introduced me to the hospital setting, where I recognised the need for trauma-informed art therapy for children with long-term physical health conditions.
I completed my professional doctorate soon after joining, researching the impact of poverty in art therapy for children and young people. Since then, my post-doctoral research has focused on art therapy in paediatric rheumatology and other medical settings.
I am part of a collaborative research group of art therapists, consultants, clinical nurse specialists and academics. The research group is a university–hospital partnership dedicated to building the evidence base for art therapy in paediatric healthcare, where psychosocial support is essential but often under-resourced.
A typical day at work in a hospital
I provide both individual and group art therapy for children and young people with rheumatic conditions who require regular blood tests and injections as part of their treatment. I carry a regular caseload and my role is fully integrated within the multidisciplinary team, working closely with doctors, nurses, psychologists, physiotherapists, youth workers, and other healthcare professionals to support psychosocial wellbeing.
A typical day might include offering five art therapy sessions to children and young people with appointments in the Outpatients Department, on the ward, in clinic rooms, or online and also attending a multidisciplinary meeting where I do focused work around preparing for hospital appointments, barriers to taking medication, developing coping strategies for blood tests or thinking about the emotional impact of a diagnosis.
One of the aspects I value most is collaborating with children and young people, recognising that they are the true experts in their diagnosis, treatment, and lived experience.

What I love about what I do
One of the aspects I value most is collaborating with children and young people, recognising that they are the true experts in their diagnosis, treatment, and lived experience. It is deeply humbling when they share their knowledge and insight, teaching me what life with a long-term condition is really like. I see my role as helping to convey their experiences and perspectives to the wider rheumatology team so that the emotional and social dimensions of care are understood alongside the medical.
I feel proud when a child or young person reaches a therapeutic goal, whether that means speaking more confidently about their diagnosis, tolerating medication and its side effects, or discovering effective coping strategies for blood tests. These moments of growth and connection make the work deeply meaningful.
A young person, Christine*, gave this perspective on their art therapy sessions:
“Last year, I was referred to art therapy by the Royal Hospital for Children Glasgow’s rheumatology department when I was having a ‘flare up’ of my condition. I was attending a lot of hospital appointments every week. I was finding it hard to communicate with the doctors and nurses but when I went to art therapy, this completely changed.”
“I enjoy coming to art therapy to see Patricia as it is the only time I don’t feel scared to come to the hospital. Patricia understands how I feel, and she can communicate to the doctors and nurses if I need it. Having someone to talk to whilst doing art to express my feelings was amazing. I had a lot of questions for the rheumatology team, but I just didn’t know how to get them across. My art therapist Patricia is amazing. She has not only made me feel more confident about coming to hospital but has also helped me share my views to the doctors and nurses.”
In previous roles, I rarely had the opportunity to witness a child’s progress beyond a block of art therapy. In this role, although the work is often short-term, I feel privileged to stay connected with many of the young people I’ve supported, as they often remain under the rheumatology team or are cared for by other hospital specialties. Having worked here for over ten years now, I see many familiar faces in the corridors. This continuity offers a rare opportunity to accompany children and families through their longer journeys, building trust and providing emotional support during what can be very challenging times.
How I look after myself in my role
I have regular clinical supervision and supportive colleagues at both Teapot Trust and the hospital. There are revitalising spaces around the site, including the Teapot Trust Elsewhere Garden, a beautiful green area offering a quiet moment of calm. I enjoy walking between clinics, greeting colleagues, and catching up with other Teapot Trust art therapists based on site.
Hospital work can be fast-paced, so I prioritise breaks, eating lunch, staying hydrated and getting plenty of steps in as I move between clinics and wards.
Emotional wellbeing supports engagement in treatment and helps young people feel more confident and connected in their care.
What I wish I had known when I started
When I first began working in the children’s hospital, I had to learn how to adapt art therapy sessions to an approach suited to a medical setting. The most helpful parts of this learning process were shadowing clinic appointments and observing how children and young people interacted with their nurses and doctors. I also spent a lot of time familiarising myself with the range of conditions, medications, and treatments used in rheumatology.
My ongoing learning is supported by attending training courses, MDT meetings, and medical conferences. However, the children and young people themselves remain my greatest teachers, each one shows me what their condition means to them personally and how it shapes their day-to-day lives.
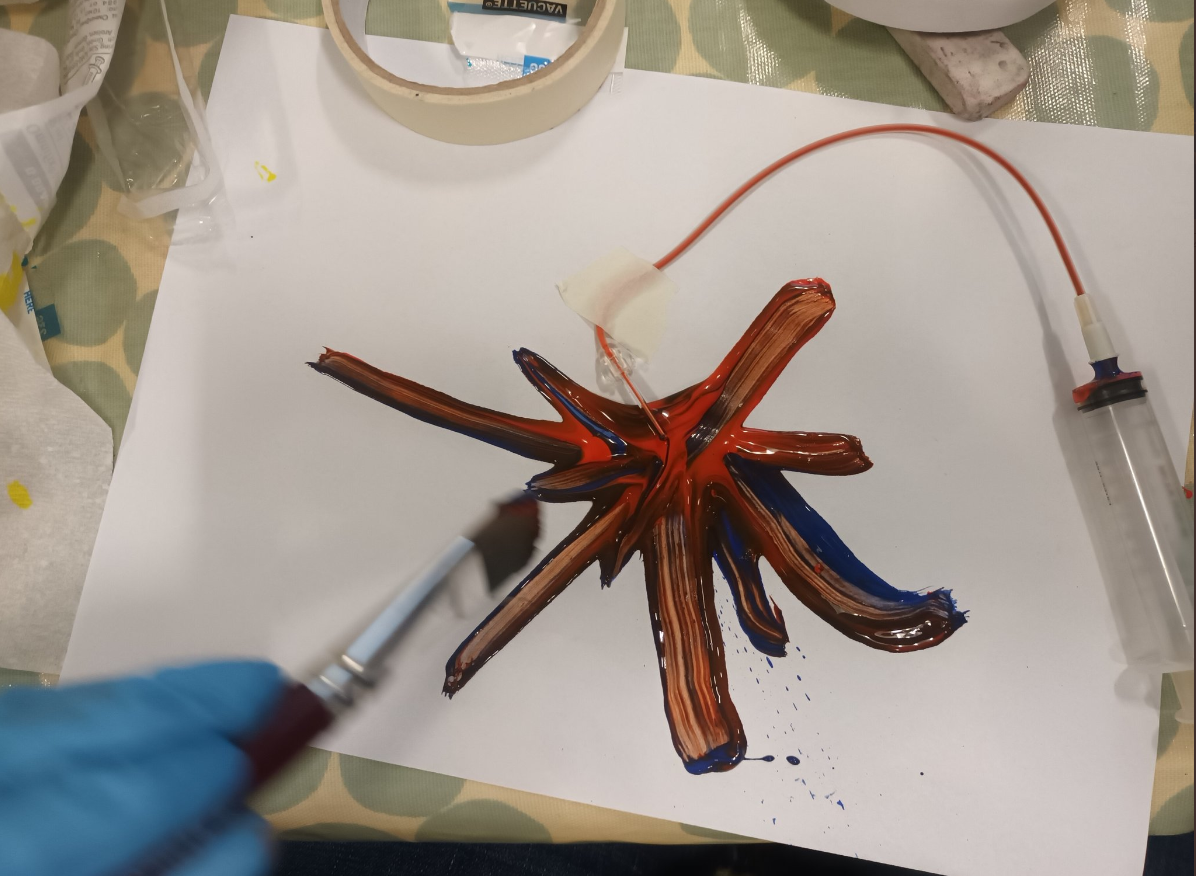
These experiences have enabled sessions to remain meaningful despite my not having a medical background. In fact, this often works to my advantage: I’m not seen as part of the medical team or as a threat, even when we use clinical equipment, such as needles or syringes as part of the art therapy process.
Children and young people frequently tell me that they find it especially helpful to explore medical apparatus within art therapy, because they can encounter these objects in their own time, in a space that is about creativity rather than examination or treatment.
Art therapy offers them an aspect of their hospital journey that they can control, and many of them tell me regularly that it is their favourite part of coming to the hospital.
Moving forward
Art therapy has an important role to play at every stage of a child or young person’s journey, from diagnosis through to transition to adult services. Emotional wellbeing supports engagement in treatment and helps young people feel more confident and connected in their care.
While the evidence base is still developing, practice experience and feedback from the children, young people and their families highlights the value of creative, psychosocial interventions within paediatric healthcare. I hope to see more art therapists being fully integrated within multidisciplinary paediatric teams, contributing to research, service development and the holistic wellbeing of children and families.
Read more
You might also be interested in reading these articles by Patricia published in our journal:
- GAIN group art psychotherapy for children: a service evaluation and acceptability study
- Developing online group art psychotherapy for children with long-term health conditions
- Art therapy and poverty: examining practitioners’ experiences of working with children and young people in areas of multiple deprivation in West Central Scotland
*Christine is a pseudonym to safeguard anonymity.
